Diabetes Medication: What Works, What to Avoid, and How It Connects to Your Skin
When you take diabetes medication, a prescribed treatment to lower high blood sugar levels. Also known as antihyperglycemic drugs, it helps your body use insulin better or make more of it. This isn’t just about numbers on a glucose meter—it’s about how your whole body, including your skin, reacts. Many people don’t realize that the same drugs that keep blood sugar in check can cause dryness, rashes, or slow-healing sores. That’s why knowing what’s in your medication matters, especially if you’re dealing with skin issues.
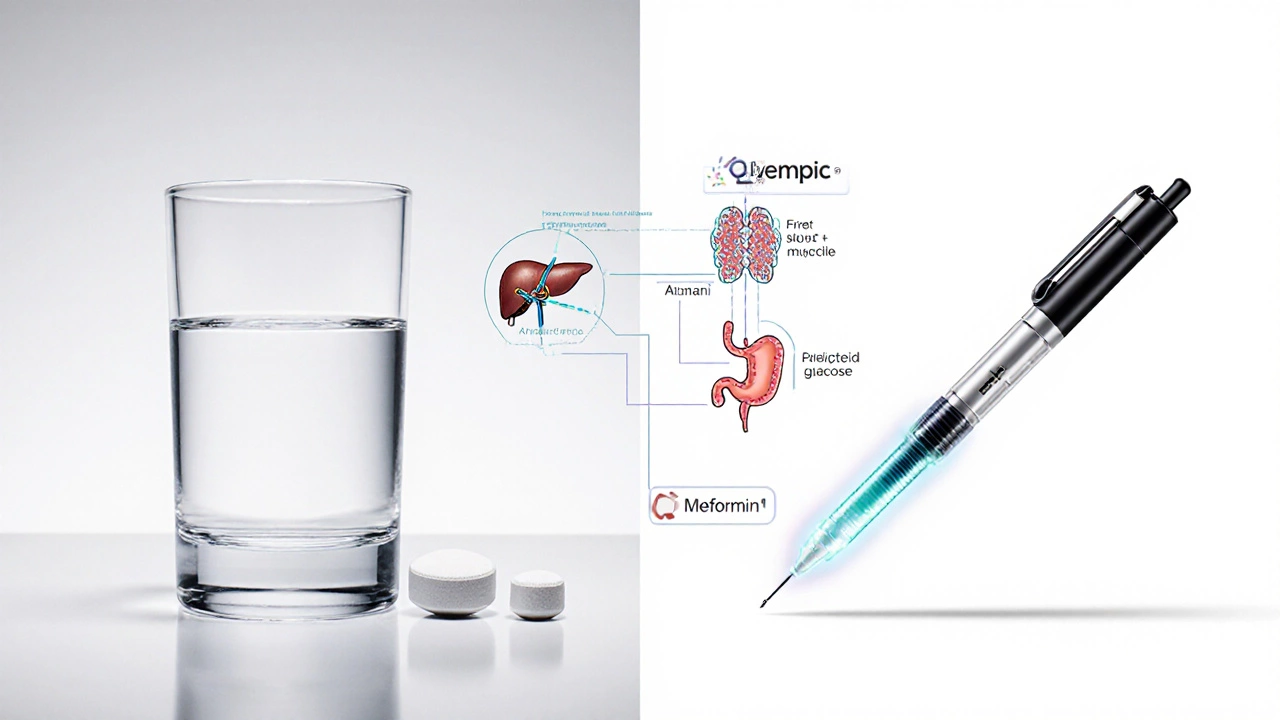
Two of the most common diabetes medications, oral drugs and insulin injections used to manage type 2 and type 1 diabetes. Also known as antidiabetic agents, they include metformin, a first-line oral drug that reduces liver sugar production and improves insulin sensitivity. Also known as Glucophage, it and insulin, a hormone therapy that lets cells absorb glucose from the blood. Also known as injectable glucose regulator, it. Metformin is often gentle on the skin, but some users report a metallic taste or vitamin B12 deficiency—which can lead to nerve damage and tingling in hands and feet. Insulin, on the other hand, can cause fat buildup under the skin at injection sites, or even allergic reactions that look like hives. These aren’t rare side effects—they’re common enough that dermatologists see them weekly.
Some newer drugs like semaglutide, a GLP-1 receptor agonist that slows digestion and reduces appetite. Also known as Ozempic or Wegovy, it are gaining popularity for weight loss, but they come with their own skin risks: nausea, vomiting, and sometimes severe itching or rash. If you’re using one of these and notice unexplained skin changes, it’s not just coincidence. Your skin is a mirror for what’s happening inside. High blood sugar weakens your skin’s barrier, slows healing, and makes infections like fungal rashes or boils more likely. The right medication can help—but only if you’re watching for signs your skin is reacting.
There’s no one-size-fits-all diabetes medication. What works for your neighbor might cause problems for you. That’s why tracking your skin along with your blood sugar is just as important as checking your numbers. Some people find their eczema improves once their glucose levels stabilize. Others notice acne flare-ups after starting a new pill. These aren’t random—they’re clues.
Below, you’ll find real stories and science-backed insights about how diabetes medications affect your body—not just your blood sugar, but your skin too. From side effects you might not know about to how to tell if a rash is drug-related or something else, these posts give you the facts you need to ask better questions and protect your skin while managing your condition.