Medication Decision Checker: Metformin vs. Ozempic
This tool helps you understand which diabetes medication might be most appropriate for your situation based on your diabetes management needs, weight loss goals, and insurance coverage. Note: This is not a substitute for medical advice. Always consult with your doctor before making any changes to your treatment plan.
How is your blood sugar currently controlled?
How much weight do you need to lose?
Do you prefer pills or injections?
How important is cost to you?
Do you have a history of kidney issues?
Answer the questions above and click "Get My Recommendation" to see which medication may be best for you.
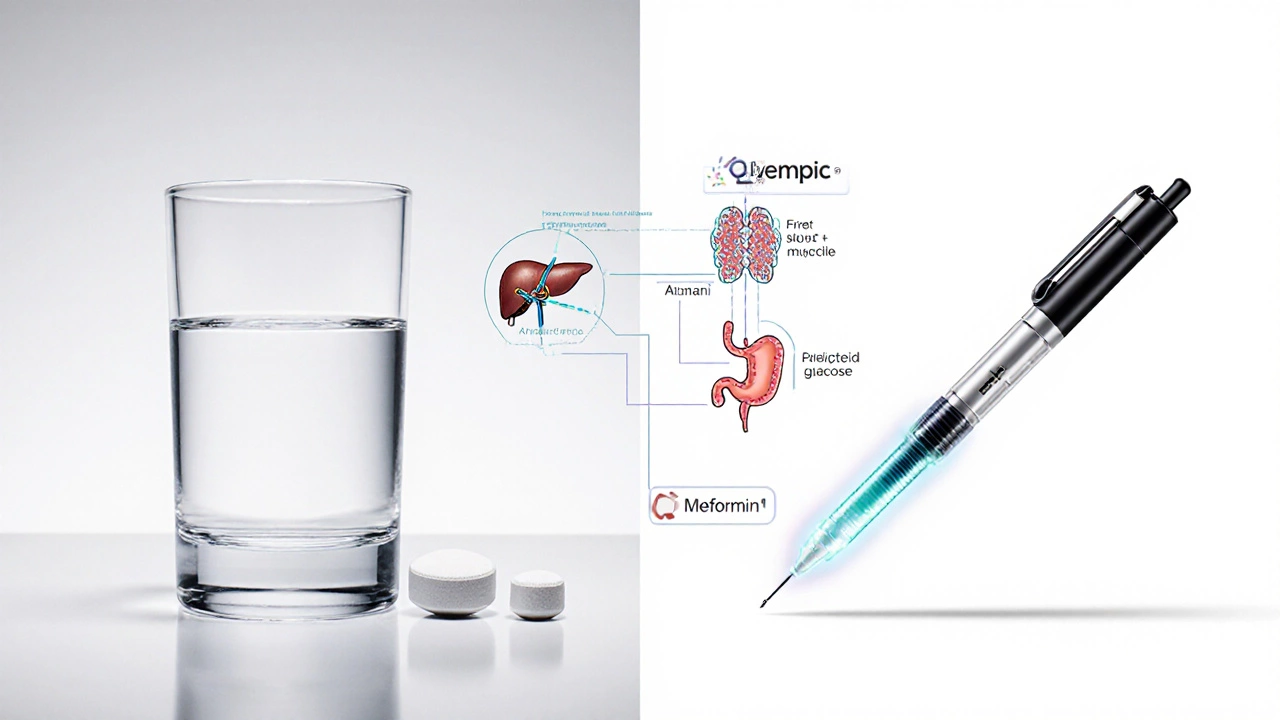
People often ask if metformin and Ozempic are the same because both are used to treat type 2 diabetes-and both can help with weight loss. But they’re not interchangeable. One is a 50-year-old pill that changed how doctors treat diabetes. The other is a newer injection that made headlines for its weight loss effects. Understanding the difference matters because mixing them up could lead to wrong expectations, side effects, or even dangerous choices.
What is metformin?
Metformin is a biguanide drug first approved in the U.S. in 1994, though it’s been used since the 1950s in Europe. It’s the first-line treatment for type 2 diabetes worldwide. The metformin is an oral medication that reduces glucose production in the liver and improves insulin sensitivity in muscle cells. Also known as Glucophage, it’s been prescribed to over 120 million people globally.
It doesn’t cause weight gain. In fact, most people lose 2 to 4 pounds on average, though some lose more. It also lowers A1C levels by about 1 to 2 percentage points. Unlike some other diabetes drugs, metformin rarely causes low blood sugar unless taken with insulin or sulfonylureas.
Side effects are usually mild: stomach upset, diarrhea, gas. These often fade after a few weeks. Taking it with food helps. A rare but serious risk is lactic acidosis, which happens in less than 1 in 10,000 patients-mostly in those with kidney problems.
What is Ozempic?
Ozempic is a once-weekly injectable medication containing semaglutide, a GLP-1 receptor agonist. It was approved by the FDA in 2017 for type 2 diabetes and later in 2021 for chronic weight management under the brand name Wegovy.
GLP-1 agonists work by mimicking a natural hormone that tells your pancreas to release insulin when blood sugar rises. They also slow stomach emptying, reduce appetite, and signal fullness to the brain. That’s why people on Ozempic often lose 10 to 15% of their body weight-sometimes more.
Studies show Ozempic lowers A1C by 1.5 to 2%, similar to metformin, but its weight loss effect is far stronger. In one trial, patients lost an average of 15 pounds over 68 weeks just from the diabetes dose. Higher doses used for weight loss (like Wegovy) led to 20+ pound losses.
Side effects include nausea, vomiting, constipation, and decreased appetite. These usually improve over time. There’s a black box warning for thyroid tumors in rodents-though no proven link in humans. People with a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia should avoid it.
How do metformin and Ozempic work differently?
Metformin works mostly in the liver and muscles. It doesn’t boost insulin. It just makes your body use insulin better and cuts down on sugar production. Think of it like cleaning up a messy kitchen-you’re not adding more cooks, you’re just making the ones you have more efficient.
Ozempic acts like a messenger. It talks directly to your pancreas, brain, and stomach. It tells your pancreas: "Release insulin only when needed." It tells your brain: "You’re full." And it tells your stomach: "Slow down." It’s more like hiring a new manager to run the whole operation.
This difference explains why Ozempic causes more weight loss. Metformin might help you lose a few pounds by reducing hunger slightly. Ozempic turns down your appetite like a thermostat. You simply don’t feel as hungry.
Can you take them together?
Yes, many people take both. Doctors often start patients on metformin because it’s cheap, safe, and effective. If blood sugar stays high after a few months, they add Ozempic. This combo is common and well-studied.
A 2023 study in The New England Journal of Medicine showed that people on metformin plus semaglutide (the active ingredient in Ozempic) lowered their A1C more than those on either drug alone. They also lost more weight-on average, 18 pounds over 6 months.
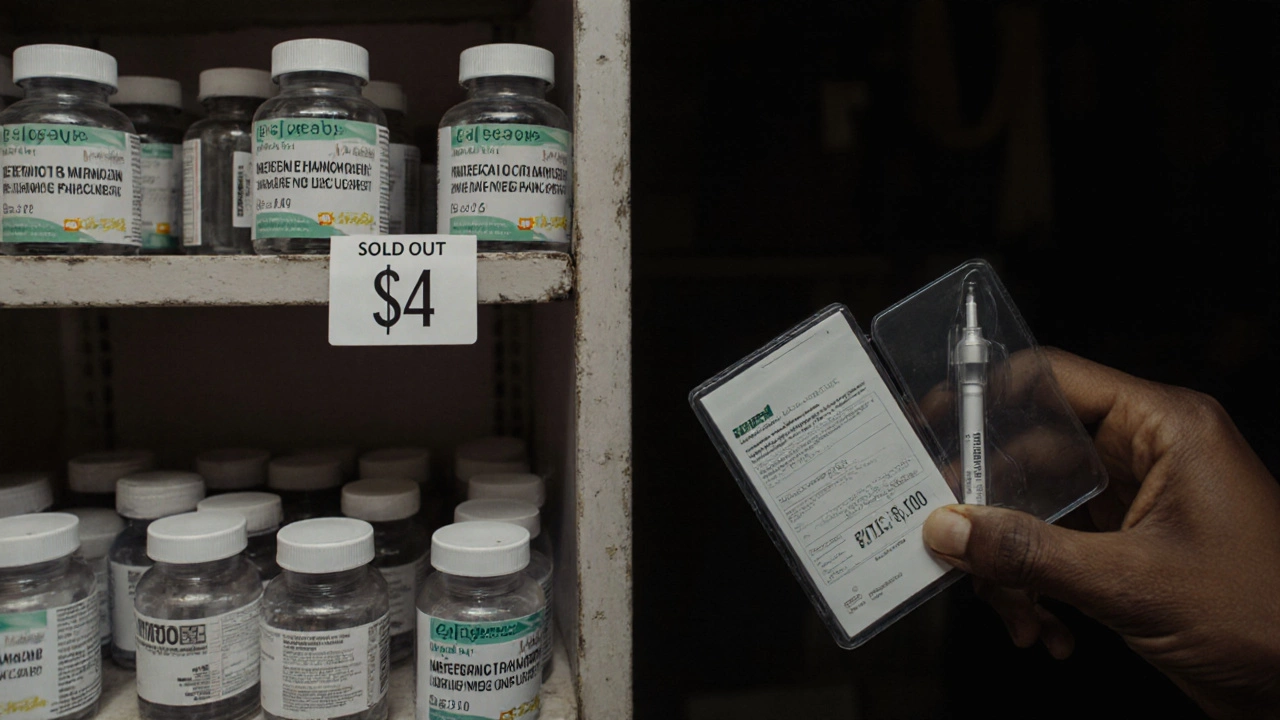
But it’s not automatic. Insurance often requires you to try metformin first. Ozempic costs over $1,000 a month without coverage. Metformin can be under $10 for a 30-day supply.
Which one is better for weight loss?
If your main goal is weight loss, Ozempic is far more effective. But it’s not the same as weight-loss drugs like Wegovy. Ozempic is FDA-approved for diabetes, not obesity. The dose for diabetes is lower than for weight loss.
Wegovy, which has the same active ingredient as Ozempic, uses higher doses specifically for weight management. Some people switch from Ozempic to Wegovy once they’ve lost weight and want to keep it off.
Metformin helps with weight too-but modestly. It’s not a magic pill. You still need to eat well and move. Ozempic does the heavy lifting for you.
What about cost and access?
Metformin is generic. You can get it for $4 to $10 a month at most pharmacies. It’s covered by nearly every insurance plan.
Ozempic is brand-name only. Even with insurance, co-pays can be $50 to $250 a month. Without insurance, it’s $1,000 to $1,300. Some patients get it through patient assistance programs, but shortages have made access harder since 2022.
Wegovy, the weight-loss version, is even harder to get. Pharmacies often run out. Insurance rarely covers it unless you have obesity and other health conditions.

Who should take which?
Metformin is best for:
- People newly diagnosed with type 2 diabetes
- Those who want a low-cost, daily pill
- People with mild insulin resistance and no major weight issues
- Those who can’t tolerate injections
Ozempic is best for:
- People who need stronger blood sugar control
- Those with obesity or significant weight to lose
- Patients who didn’t respond well to metformin alone
- People okay with weekly injections and willing to pay more
Many end up on both. There’s no shame in that. It’s not failure-it’s smart management.
What happens if you stop?
Stopping metformin? Blood sugar usually creeps back up over weeks. Weight may return slowly, especially if diet and activity don’t change.
Stopping Ozempic? Blood sugar rises faster. And weight often comes back-sometimes all of it-within 6 to 12 months. That’s because Ozempic’s effect on appetite fades quickly. It doesn’t retrain your body; it temporarily suppresses hunger.
This is why long-term use is often needed. It’s not a cure. It’s a tool. Like blood pressure meds, you may need it for years.
Final takeaway
Metformin and Ozempic are not the same. One is a low-cost, old-school pill that improves how your body handles sugar. The other is a powerful injection that changes how your brain and stomach respond to food. They can work together. But they’re not interchangeable.
If you’re wondering which one is right for you, talk to your doctor. Don’t switch based on TikTok trends or celebrity stories. Your health isn’t a viral post. It’s a long-term plan-and the right tool depends on your body, your goals, and your life.
Can metformin cause weight loss?
Yes, metformin can lead to modest weight loss-typically 2 to 4 pounds on average. It doesn’t directly burn fat, but it reduces appetite slightly and improves insulin sensitivity, which can help prevent fat storage. Some people lose more, especially if they combine it with diet and exercise. But it’s not a weight-loss drug like Ozempic.
Is Ozempic just for weight loss?
No. Ozempic is FDA-approved for treating type 2 diabetes. Its weight loss effect is a bonus. The version approved specifically for weight loss is called Wegovy, which uses higher doses of the same active ingredient. Ozempic doses are lower and meant for blood sugar control.
Can I switch from metformin to Ozempic?
Yes, many people do. Doctors often start with metformin and add Ozempic if blood sugar stays too high. You don’t need to stop metformin right away-often both are used together. But never switch on your own. Ozempic requires a prescription and careful dosing to avoid side effects like nausea or low blood sugar.
Why is Ozempic so expensive?
Ozempic is a brand-name drug with no generic version yet. It’s made by Novo Nordisk and uses complex biotechnology to produce semaglutide. Manufacturing costs, patent protection, and high demand have driven prices up. Even with insurance, out-of-pocket costs can be high. Some patients get help through manufacturer coupons or patient assistance programs.
Do I have to take Ozempic forever?
Not necessarily, but stopping often leads to weight regain and higher blood sugar. Ozempic doesn’t fix the root cause of diabetes-it manages symptoms. If you stop, your body returns to how it was before. Many people stay on it long-term, similar to how people take blood pressure or cholesterol meds. The goal is to improve health, not just take a pill.
Can I take Ozempic if I don’t have diabetes?
Ozempic is only approved for people with type 2 diabetes. For weight loss without diabetes, the FDA-approved version is Wegovy. Off-label use of Ozempic for weight loss is common but not officially recommended. Always consult your doctor before using any medication outside its approved use.